PSY-PGx
A New Intervention for Implementation of Pharmacogenetics in Psychiatry
About the project
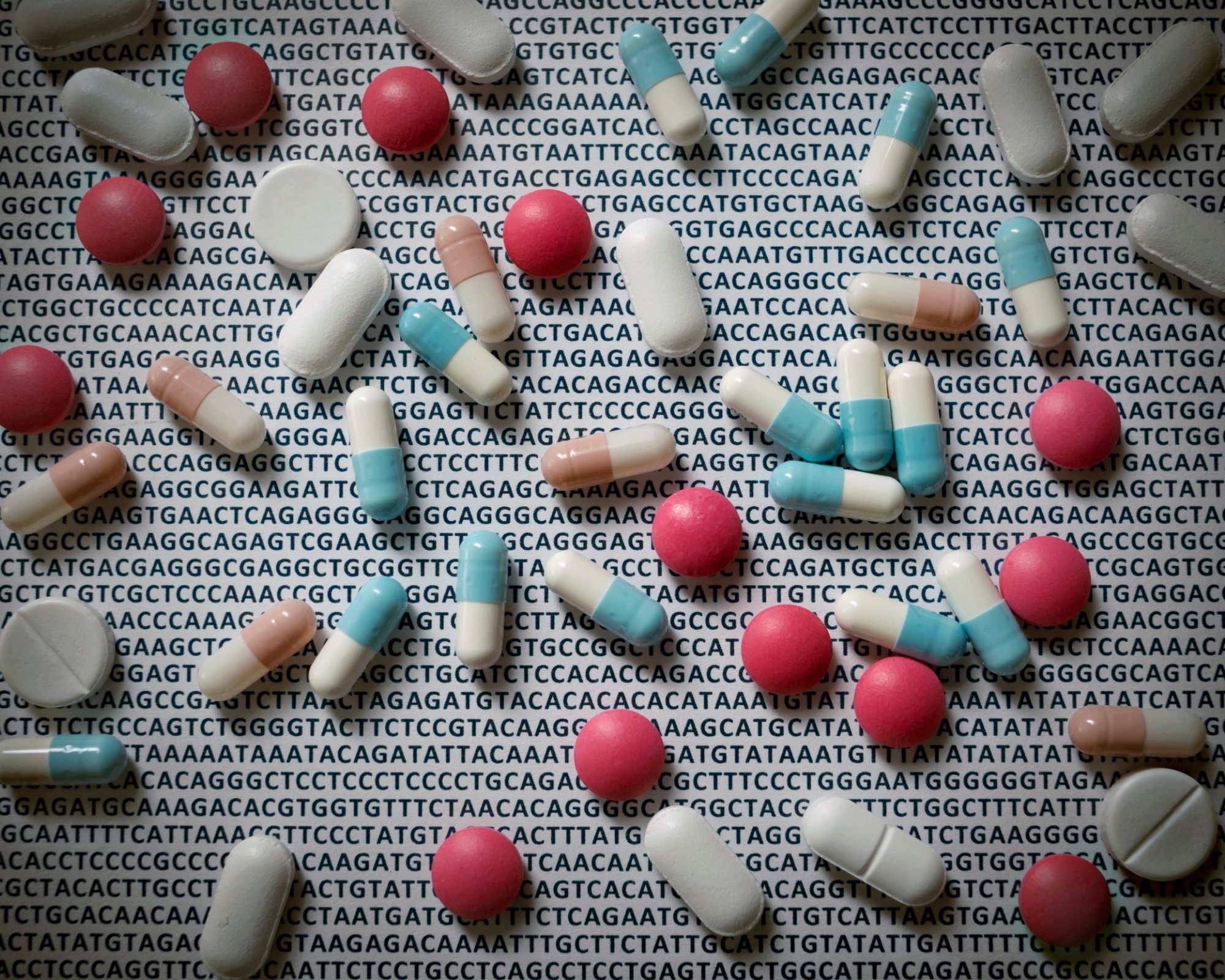
Due to the chronic relapsing nature of mental disorders and increased life expectancy, the societal burden of these non-communicable diseases will increase even further. Treatments for mental disorders are available, but their effect is limited due to patients’ (genetic) heterogeneity, low treatment compliance and frequent side effects. Only one-third of the patients respond to treatment. Today, medication selection in psychiatry relies on a trial-and-error approach based mainly on physicians’ experience. Pharmacogenetic testing enables assessing person-specific genetic factors that predict clinical response and side effects. Recent studies show that genotyping of drug-metabolizing enzymes can increase the effectiveness of treatment, which could benefit millions of patients. PSY-PGx is the first initiative to propose a large-scale non-industry sponsored clinical study that demonstrates the clinical benefits and potential of implementing pharmacogenetics for psychiatric patients in existing medical settings. To this end 1) available biobank data (www.biobankki.fi, www.ukbiobank.ac.uk), with the aid of AI, will be searched for pharmacogenetics that influence medication response. This information is used to 2) perform a clinical trial that will be the first large international, multicenter clinical trial on using pharmacogenetic-based treatment personalization in real-life psychiatric care for depressed, anxiety or psychotic disorder patients. All data is combined with AI to set-up an algorithm for personalizing medication prescription for psychiatric patients that reduces side effects and increases effectiveness of pharmacotherapy. PSY-PGx will thus deliver a new model of care for sustainable healthcare systems and reduce the suffering of psychiatric patients.
An article introducing the project: Large-scale study aims at personalising medication in psychiatry
As many as two thirds of all psychiatric patients do not respond well to treatment with drugs. While compliance and frequent side effects play a major role, there are also genetic variations which determine whether serious side effects occur, and which can also prevent medication from working. An international consortium led by Dr Roos van Westrhenen (Maastricht University/Parnassia) is to conduct a pharmacogenomic study to establish the relationship between response to treatment and genetic background. This will make it possible to individually tailor the drugs prescribed to psychiatric patients, and thus make therapy more effective. The research was recently awarded eight million euros in European funding.
Pharmacogenomics
Due to the chronic and recurring nature of psychiatric disorders, paired with overall increasing life expectancy, the social burden of mental illness will only continue to increase. This development shows the need to make medication in psychiatry more effective. Pharmacogenomics is the field that aims to use a knowledge of variations in human DNA to explain why medicines cause many side effects in some people and/or show little or no efficacy in others. Variations in DNA can lead to differences in the activity of proteins that enable the body to absorb drugs. Although pharmacogenomics is increasingly being applied in the Netherlands, for example in oncology, until now it has hardly been used in psychiatry. ‘Medication is often prescribed in psychiatry through a trial-and-error approach, mainly based on the experience of doctors,’ says lead researcher Roos van Westrhenen. ‘Recent studies show that determining genes involved in drug metabolism can increase the effectiveness of treatment. Millions of patients can benefit.’
Therapy
The international consortium, which apart from Maastricht University also includes the University of Groningen and the mental healthcare provider Parnassia Groep, will use artificial intelligence to map pharmacogenomic characteristics. At the same time, it will conduct a large-scale clinical study among people suffering from depression, psychosis, or anxiety, again using artificial intelligence to create an algorithm to personalise drug prescriptions, thus reducing side effects and increasing efficacy. ‘This research will form an important basis to tailor drug therapy more closely to the individual,’ says Professor Bart Rutten, head of the Department of Psychiatry at Maastricht UMC+, one of the centres participating in the clinical study. ‘It thus offers promising prospects to reduce mental suffering among patients.’
DONATIONS